Gender Affirming Surgery and IBD
As always, this will be specific to your IBD and transition journey and requires a conversation with your gastroenterologist, colorectal surgeon, and gender-affirming surgeon. For individuals with fistulizing disease (Perianal, rectal, and preexisting pelvic floor disorders (eg, Crohn’s disease, prior radiation, prior trauma, and so forth) ,this may impact the tissue quality needed for reconstruction can affect your candidacy for all genital gender affirming surgery (phalloplasies, vulvoplasty, etc.This is why it’s VERY important to let your doctor know if you notice any changes in your IBD or discomfort so you can have achieve your transition related goals!
Close communication between your gastroenterologist, colorectal and gender-affirming surgeon, and radiologists is critical. Please do not ever feel hesitant to speak up if you feel something is not your 'normal'.This is not to be doom and gloom!! Many transgender people with IBD have had successful gender-affirming surgery - it is just VERY IMPORTANT that you keep all of your doctors and surgeons in the loop.As with most LGBTQ+ health topics in IBD, there is very limited research and information regarding gender affirming surgery and IBD. It may be helpful to reach out to IBD doctors with training or speciality in LGBTQ+ health for help. Together we will figure it out!
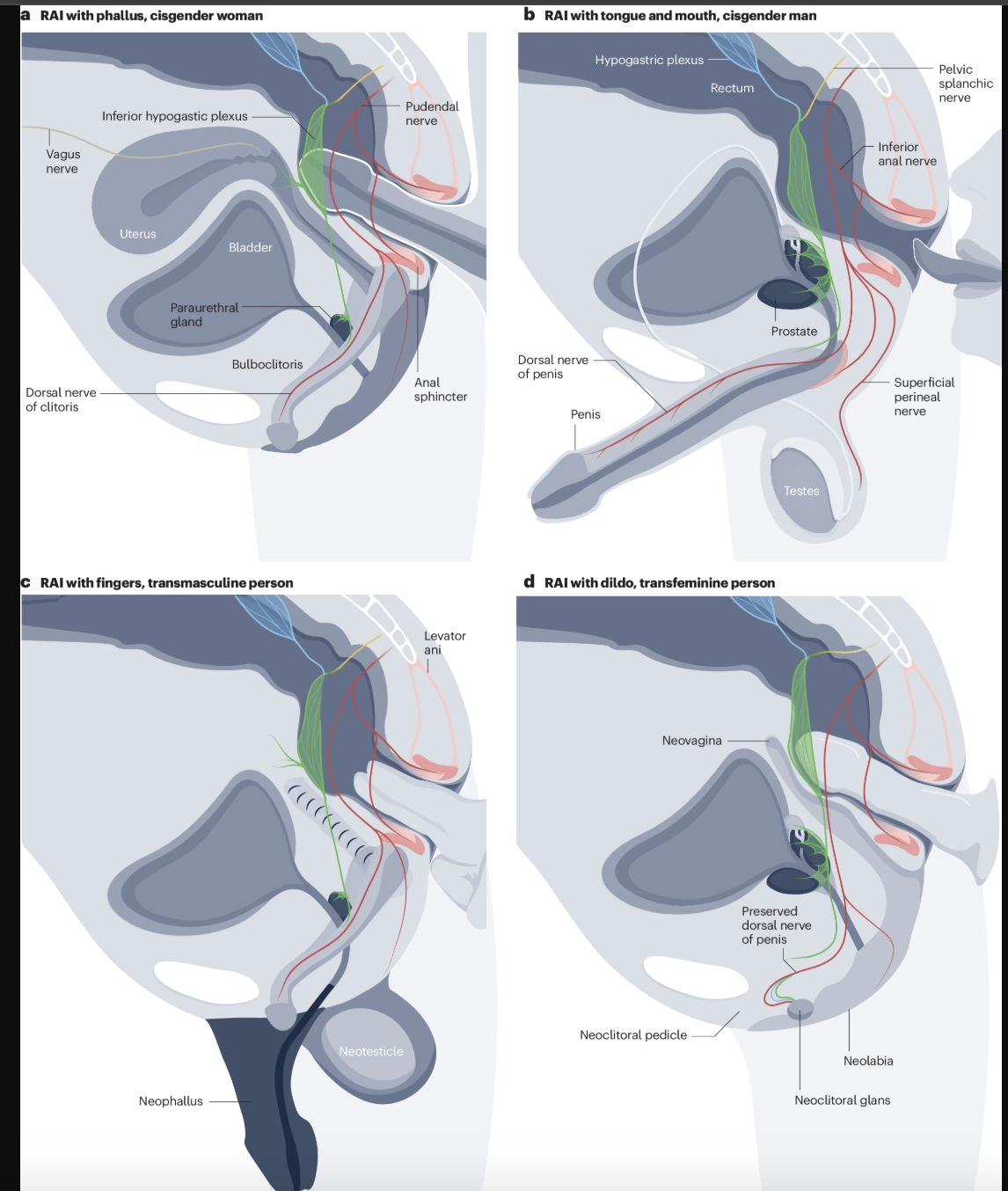
Examples of genitopelvic anatomy of transgender individuals with IBD after gender affirming surgery and/or gender affirming hormone therapy (testosterone leading development of neophallus